How to tell if you have pelvic congestion syndrome and when to seek help
Pelvic congestion syndrome (PCS) is a frequently overlooked cause of chronic pain in women, often mistaken for other conditions.
Recognising the symptoms early is crucial for effective treatment.
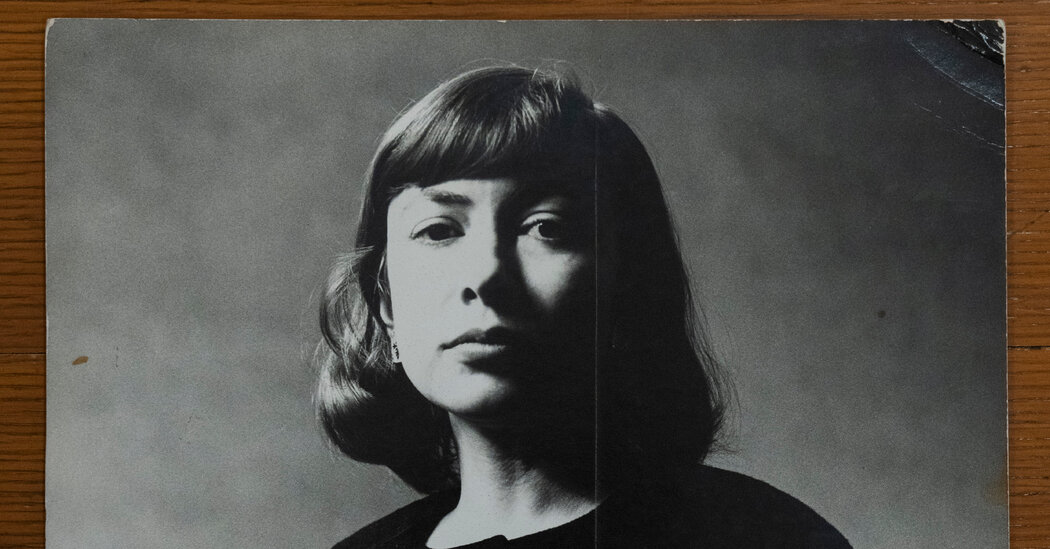
Dr Sophie Strong, consultant gynaecologist at The Pelvic Pain Clinic at The Whiteley Clinic, sheds light on this often misdiagnosed condition.
PCS, also known as pelvic venous insufficiency, stems from faulty blood flow in the pelvic veins.
“The easiest way to think about it is they’re essentially varicose veins which are inside the pelvis,” explains Dr Strong.
These veins, similar to varicose veins in the legs, become dilated and dysfunctional, leading to a persistent aching or dragging sensation.
Because these veins are internal, specialist scans are necessary for diagnosis.
While more common in women, PCS can also affect men. The Whiteley Clinic emphasises the importance of raising awareness about this condition to ensure timely diagnosis and appropriate management.
What causes it?
“When you have a varicose vein, that valve is not working properly, so what happens is that all of the blood kind of pulls and it fills and stretches the vein, and that creates heaviness, tenderness and pressure,” explains Dr Strong.
Varicose veins tend to run in families, but there are other risk factors, including pregnancy.
You’re more likely to have PCS if you’re between ages 20 to 45 and have given birth more than once, according to the Cleveland Clinic.
“Pregnancy can put a big pressure on the vein system, and that’s because your body is carrying so much more blood around, and you have a very large mass that’s filling your pelvis, which affects the way that the valves and the veins work with returning that blood to the heart,” explains Dr Strong.
What are the most common symptoms of PCS?
The symptoms people experience depend on the location of the faulty veins, but the hallmark sign is chronic pelvic pain.
“If the ones around the womb and the uterus are not working properly and become very heavy and baggy, that can give a real sensation to chronic pelvic pain,” Dr Strong says.

“It can make periods painful, and we also see people presenting with pain having sex, or even pain after sex, because you’re essentially contacting an area which is sore and bruised and is competing for space.”
The Cleveland Clinic website also states that other common symptoms include frequent bouts of diarrhoea and constipation (irritable bowel), peeing accidentally from laughing, coughing or other movements that stress your bladder (stress incontinence) and / or pain when you pee (dysuria).
And, for some, the varicose veins are very visible around the vagina and the vulva.
“Sometimes they look like little blue to black grape-looking structures,” adds Dr Strong.
Why is it important to get diagnosed?
“Unfortunately, varicose veins don’t get better by themselves, so unless they are picked up, diagnosed and treated, they will only get worse,” says Dr Strong.
“What we see is the sooner that you detect these veins are not working properly, then the sooner you can get treatment earlier to stop them from getting so bad.”
GPs are usually the first point of call, and then you might be referred to a specialist.
“Typically [in our clinic] a patient would come and have an appointment with a consultant, who would take a full history from them and examine them, and then they would have a specialist scan called a duplex ultrasound scan,” explains Dr Strong.
“We use a transvaginal duplex ultrasound scan, an internal vaginal scan, where we measure the blood flow through each of the different veins within the pelvis to identify the ones that aren’t working properly, and that can then tell you which veins need to be treated.”
Can it be treated?
One is the most common treatments for PCS is pelvic vein embolisation.
“This is a walk-in-walk-out procedure which involves carefully placing tiny little coils, thinner than human hair, inside the damaged veins under X-ray guidance,” describes Dr Strong.
“The coils cause a local reaction inside the veins over time, causing it to close itself off. This therefore blocks the pathway that wasn’t working and allows the other healthy veins inside the body to take over returning the blood to your heart in a more streamlined way.
“The normal veins work much more efficiently and do not cause pain as they do not have any reflux.”